Introduction
The thickness of your cornea will be taken into account when your doctor assesses your eyes for refractive surgery. Your age, level of refractive error, and the existence of keratoconus, an eye condition, are all factors that the majority of specialists will consider. The corneal thickness that remains after having LASIK performed on your eyes will subsequently be calculated by him or her to establish eligibility.
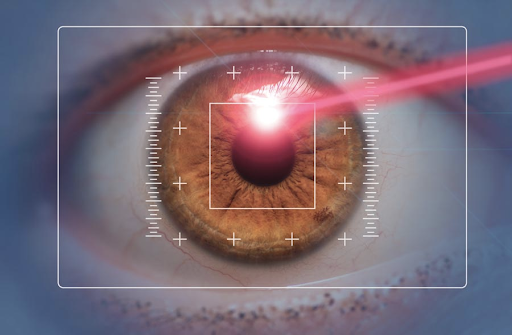
What is the necessary corneal thickness required for Contoura Vision?
The minimum central corneal thickness you should have is 500 microns. While a corneal thickness of 485 m, which was formerly regarded to be the cutoff for LASIK, may be normal, you won’t be approved for the procedure unless you don’t have forme fruste keratoconus, skew deviation, or keratometric readings higher than 47.00 D. Advanced examinations of your cornea’s form, known as corneal topography, are used to determine these. You won’t be a good candidate for the operation in this circumstance. When the corneal thickness is 495 microns and more, advanced bladeless refractive procedures like Contoura Vision and Femto bladeless LASIK may be used (specs power of maximum -8 can be corrected).
Surface ablation procedures like PRK and ASA may be carried out on corneas with a thickness of 450–495 microns. You may also choose to have ICL surgery, which includes the implantation of lenses if your budget permits. For those whose corneal thickness is less than 450 microns, ICL surgery is still the only choice. Patients who had Sub Bowman Keratomileusis, SBK, or LASIK with a corneal thickness of 485 m did not have an increased risk, according to studies. As surface ablation either avoids the need for a corneal flap or produces a flap that only contains the epithelium and not the stroma and is thus thinner, it is often mentioned as a therapeutic option for thin corneas. As a result, the remaining corneal bed may be thicker than it would be after a standard LASIK procedure, although many experts think that the cornea is just as robust after SBK as it is following surface ablation.
How does a 460-micron corneal Lasik treatment work?
The surgery called “No LASIK” would be that.
In addition to being too thin for LASIK, 460 microns is indicative of a condition that is contraindicated for the procedure, such as keratoconus.
Moreover, standard PRK is not recommended. Nevertheless, it is possible to combine PRK with collagen cross-linking or CXL, either with or without InTacs intracorneal ring segments. The ICL and other phakic lenses, as well as refractive lens exchange(RLE), are additional possibilities to the keratorefractive surgeries mentioned above. Any of them should be carried out by a surgeon who has a lot of experience doing the corresponding operation. What occurred when someone attempted that, we can tell you.
They developed keratoconus, a disorder that causes extreme blurriness in the eyes that is unaffected by glasses. In connection with this, there have been some suicides.
It may be feasible to achieve a clear vision, but only with the use of specially manufactured contacts or, in certain circumstances, corneal transplants.
LASEK may be an option for those with corneas that are too thin for LASIK. You should always keep the cornea’s outer layer, which ranges in thickness from 250 to 300 microns, untouchable. Your eye will look like a plastic-molded child’s camera if the cornea is any thinner and isn’t robust enough to maintain its form. You are playing Russian roulette if you ignore medical advice and look for a surgeon who will proceed with the treatment despite having thin corneas. You could be fortunate and continue to be able to see thereafter.
One has to be aware of the differences between LASIK and Surface Ablations in order to comprehend them. These treatments alter the cornea’s curvature, which focuses light onto the retina, the eye’s light-sensitive area, to correct the refractive power of the lens.
LASIK’s differences from Surface Ablation LASIK
A little flap of the cornea is raised during LASIK surgery utilizing either a mechanical keratome (traditional LASIK) or the laser itself (bladeless or blade-free or all-laser LASIK). An area of the stroma and the corneal epithelium makes up this flap. After the cornea’s stroma (component tissue) has been irritated, the laser, which is guided by a potent computer program, modifies the cornea’s surface to correct the eye’s refractive error and eliminate the need for glasses for clear vision.
- Surface Ablation
In Photorefractive Keratotomy or PRK, the uppermost layer of the cornea, known as the epithelium, is removed by the surgeon using an alcohol solution in order to reveal the stroma. Your cornea is then modified by the ophthalmologist using a laser to guarantee that you no longer need eyeglasses. Just the epithelium is taken out; it grows back over the course of three to four days without any flap being produced. A bandage contact lens is placed in the cornea by the surgeon after the SMILE surgery to preserve it until the epithelial layer has fully recovered. The thick contact lens also aids in lessening the pain that has been variously characterized as mild to severe at this period, as well as the experience of having “something” or a foreign body in the eye.
Advanced Surface Ablations, or ASA, is the term used to describe a collection of procedures that include Supra LASIK, also known as touch-less LASIK, and LASEK, in which the epithelial flap is removed using a specific microkeratome called the Epi-keratome and reinstalled at the conclusion of the treatment (which is a surface laser procedure that uses a technologically advanced excimer laser to remove the surface cells before performing the reshaping of the cornea).
The drawbacks of surface ablations, such as Supra LASIK, are as follows:
- Uncomfortable symptoms for the first two to three days after therapy until the epithelium grows back.
- Comparatively speaking to LASIK, vision recovery is slower.
- Due to the removal of the epithelium during the treatment, there is a small chance of corneal haze.
- The clear benefit of ASAs is that they are helpful for individuals who have already had corneal surgery, including corneal grafts. Experts from all around the globe are increasingly questioning the supposed benefit that they may provide to those with thinner corneas.
- Even for patients with thinner corneas, physicians prefer to provide one of the newer LASIK versions as LASIK technology advances and is better tailored to the requirements of the particular cornea.
Recommendations for Novel Techniques for Individuals with Thin Corneas
- The LASIK procedure using wavefront guidance
With the use of computerized imaging technologies, this procedure may program an excimer laser to reshape the cornea by creating an extremely accurate three-dimensional “map” of the patient’s cornea. In order to accomplish a more successful and secure vision correction than traditional LASIK, wavefront technology can evaluate extremely minute anomalies in the corneal surface by collecting 200 measurements.
- Topography using Contoura-directed LASIK
In the United States and other areas of the globe, this technique is the most recent LASIK eye surgery to get FDA approval. In contrast to other procedures (such as LASIK), it corrects vision based on the distinctive shape of the eye rather than the prescription for the wearer’s present glasses or contact lenses. In comparison, wavefront-guided LASIK, which is presently available, measures around 200 points on the cornea. It measures 22,000 points. According to this, even the tiniest form, optics, and curvature flaws in the periphery may be taken into consideration, allowing for the rectification of refractive faults with a level of accuracy never before possible.
Topography using Contoura With the use of guided LASIK technology, the computer may design a personalized treatment algorithm that manages the laser system with extraordinary precision.
Contoura Vision Topography Guided LASIK has the following notable benefits as a result of its precision and accuracy:
- Light scattering and starbursts are less common at night, making nighttime driving easier.
- lowered sensitivity to light and glare
- more clarity and quickness while reading
- better to that of glasses or contact lenses in terms of eyesight quality
- more comfortable viewing conditions, and fewer higher order aberrations
The likelihood of corneal problems, especially in thin corneas, is much decreased in the most recent iterations of LASIK since the flap’s development is so carefully managed. There is enough evidence to conclude that the patient benefits from improved postoperative comfort as well as improved eyesight and quality of life.